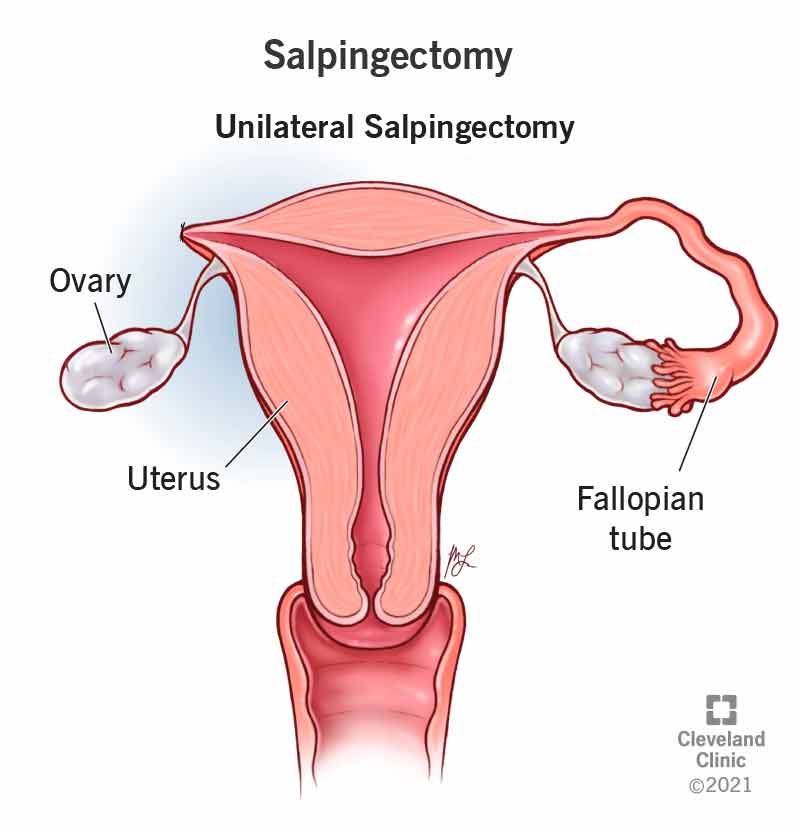
Hmm… So, it was a ectopic pregnancy that then leads to a Unilateral Salpingectomy.
Nothing to be proud of but well it happens.
So I was saying I was really upset about the first doctor who probably treated me more like a case.
I think in as much as I would want to point my finger, its pointless. 😀
One of my qualms was the idea that there wasnt enough education. I didnt know the implications if things were not followed up tightly. (If more factors had worked to my advantage, I could have gotten my treatments 1 day earlier, I believe.)
That same doctor looked me in the eye in all seriousness and mentioned that I’ll have to come back for the blood test in 48hrs time to test for the 3 possibilities. One of it being Ectopic Pregnancy, she asked me if I knew what it means.
To me, it was simply that the pregnancy was parked at the wrong position. There was no after-thoughts about it. I was fully committed to my good hope. I am pregnant, its just too early to see on the scans. It didnt occur to me that my ectopic pregnancy had implications.
Anyway, after I was sent out to draw blood, it occurred to me that 48hrs time, would mean 3pm, 2 days later. I have a lesson at 4:30pm that day. According to my understanding, theres no way I could get whatever that needs to be done, a doctor consultation, leave and be on time for my lesson. Which means I’ll have to take leave from work. Its inconvenient but not impossible.
So I went back and ask if I could come back after the lesson, the nurse went in to help me ask the doctor, she came out and ask what time it would be, I said 6:30pm. She went back in and then came out and tell me it was okay. so yeah… 51hrs+
That was Monday. Tuesday I had the bleeding episode. It didnt seem major to me. I continue to conduct my lesson. That was still within the 48hrs.
That evening’s dinner, I was telling my husband, I think the pregnancy’s definitely gone. I discharged clots. I was telling him I had no motivation to take a Grab and rush over after after work. Just take the train will do. Like there’s no rush, cos… Its lost. … Not knowing it was leading up to more than just that.
Next day, went teaching as normal, light bleeding carried on. Finally lesson ends, Went to the Urgent O&G department on GrabHitch. Was quite stunned by what I heard at the registration counter and even at the nurse’s station. They mentioned there were doctor’s notes for doctors, but they was no explanation as to why I was referred to come in to the Urgent O&G. I was very very very very upset.
It was after work, I’m tired, I’ve been bleeding, I wanna eat, I wanna rest. It already felt like the doctor treated me as a case, and then now, the nurses are telling me they need to consult in-order to order the blood test for me. That someone in there didnt want to order the blood test because they didnt know why I was asked to come to the Urgent O&G department. That mental state, that physical state + possibility of being denied medical attention after going all the way there. I was like “What in the gibberish hell is this.”
Thankfully the nurses were kind, they processed my papers, offered me a pad when I said I need to go buy and I had my blood drawn. It was already 8pm by then. I had to wait 2hours for the laboratory result, 10pm+ then wait for my turn to have doctor’s consultation. I brought marking to work on, so time flew past.
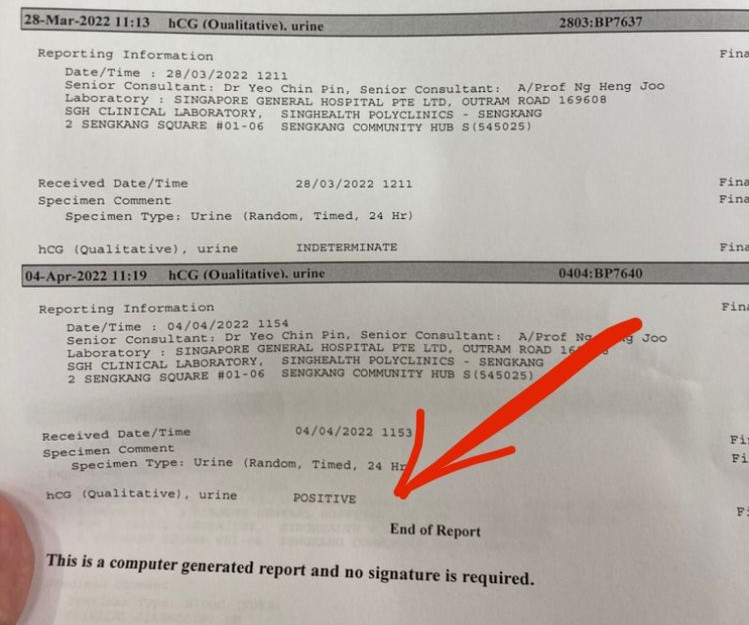
Thankfully the first Urgent O&G doctor that attended to me, she was kind to ask how I was, I said I could be better. We talked, I raised my question about SOPs, and why was it that I was almost denied medication attention, didnt pursue as I just want to move on. She asked about quantity of bleeding. Mentioned that the change in hormones level as not significant enough, had in-fact dropped (which wasnt surprising to me), 104 -> 96 (something like that) did a scan in the room. Discussed about payment as more scans are required and that since its post-working hours there’s not enough hands in the sonar-scan room, I have to wait for the scan. They instructed for me to wait outside, they felt the scan was necessary and they’ll get back to me on how to proceed next.
That was already 10pm+ pushing 11pm.. I went out, sat down, waited to be called. Then another doctor called me. Dr W. 😀 funny that they mis-cued and thought I hadnt had been consulted. 😀 Went out and waited again for the whole scan thing.
A nurse came out and spoke to me, she said theres only 1 radiographer left, and has to attend to an urgent case, I’ll have to wait at least 1.5hrs before I get my scan that evening. It didnt sit well with me… 1.5hrs (not prioritsed yet) to wait to get scanned, 2hrs for the result, then wait again to get doctor consultation. so that 3.5hrs+ with the possibility of further delay. Thats 11pm + 3.5hrs. That would lead up to 2:30am, pushing 3am.
nope, didnt sit well with me. I was too drained mentally, physically for that stretched into 3am. I told the nurse that would be 3am, I would rather come back another day. Nurse said, coming back would mean 8:30am. I was super happy with that. At least I could clock 7hrs of sleep before I could come back again.
The nurse said to wait she’ll consult with the doctor and get back to me again.
A doctor with same name as I do called me in. She mentioned that she tried to escalate the scan for me, and even consulted a senior doctor. She mentioned that the previous doctor noticed there were blood on my pelvis area. I responded saying ‘but its blood everywhere, what’s wrong with that?’ 😀 silly me. Seriously at the point of time, I still didnt understand the urgency of what I was going through.
The doctor was quite insistent on me going in for the scan and follow up with more. I was way passed tired at that point. After her pep talk, I agreed, since it seemed really important to her. I was told to wait outside.
I sat outside and waited, and then Dr W. called me in. She said there was another case that is in queue for the scan, so I’ll have to wait for 2 person to get their scans done before its my turn. and then + wait for result + consultation. Thats going to be way past 3am.
I literally said no, I’ll come the next day. Then she asked if I want to be admitted. I said no, cos I was afraid of the hospital bill and nothing seems to be deterring me from going home to rest. (The truth is I had hospitalization insurance, and if I had chose to be admitted to Ward C, the whole blood test and scan thing could just be charged to the policy and medisave, I didnt need to pay any cash upfront. I didnt know at the point of time.)
So she had me sign consent on refusal to be admitted and let me go home. I texted my boss to say I might need relief teacher the next day.
Came back the next morning 8:30am registration, with my water bottle and my battery bank.
Was ushered to the sonar-scan department, waited for my turn.
Got scanned and was told to wait to be brought back to the Urgent O&G department. The radiologist dont usually tell us anything, its the doctor who does it. A porter came with a wheelchair, and insisted on wheeling me. She was smaller-built than me, I feel so bad. I kept telling her, its okay, I can walk, I’m fine to walk. I’m too heavy for you to push. Still got wheeled to a nurse station, got my BP taken. Waited… and waited…
Was finally wheeled (again) to the Urgent O&G department and asked to lay down. Got monitored on the BP and pulse machine. Still no idea why or what was happening. The nurse who had registered me that morning noticed me and had a deep frown on her forehead as I got off the wheelchair and was getting onto the bed. “You remember me? I registered you just now.” I asked her about the frown, and said something really serious must be happening to me then..
Then Dr N. came. Asked how I was and instructed to wheel me to her office. I quickly asked if I would be able to leave in time for my early evening class that day, she said I wouldnt be able to. That was before lunch. Hastily I sent out the confirmation that I needed a relief teacher to take my class and cancelled a ShopBack customer survey.
In the office, she explained that it required urgent surgery. There’s bleeding near the foreign body and its located in the fallopian tubes. I cried soon after cos I was relieved. and I told her that I’m crying cos I have closure, I feel relieved cos I know whats happening.
She explained that there were 3 possibility, (1) ruptured ectopic pregnancy, which will then lead to a salpingectomy, (2) Tubal abortion, (3) ovarian cyst. They needed to do a laparoscopic procedure to be sure, + save the tube as it may be badly damaged + do a D&C to clean out the lining.
I asked if there was anyway to save the pregnancy or possibility that there was implantation on the lining.
She said according to the hormones level, the pregnancy is very unhealthy and will go no where.
Yeah.. so consent was given and I was told to wait outside and I’ll be brought back to the Urgent O&G and await for admin works and ward to be available while I wait for my turn to go in for emergency surgery.
I text the relevant persons, half crying, half trying to lighten the mood, half tearing, half relief, just going with the flow.
Wasnt suppose to eat or drink before the surgery. So I was put on drip.
Was finally pushed to the high dependency ward and a nurse was doing admin on the computer to do the necessary paperworks. Somewhere while waiting. I told her “dont mind me, I need to cry it out”, I didnt need her to go away, I just needed to assure her that I’m just letting it out, not that I was having a breakdown. She pulled herself away from my private space real fast. I turn to the side and pulled up a pillow. I let it out to grief and heal, real fast, 2 minutes tops? That was all I needed, to just let it out. 🙂 Probably was prepared since the very beginning, that 1st pregnancy is common to end with miscarriage, the bleeding on the Tuesday, telling the husband that I felt a clot exiting. and finally the relief to have closure.
Waited and text the family, informed the husband about the ward and bed number.
Had multiple doctors confirm my details before finally getting to the operation table.
It was only during a talk with the anesthesiologist that I realised that the reason why my feet has been cold the past few days could be because of the bleeding.
I kept complaining that my feet was cold as I entered the operation room. I remembered a doctor yelling at me to not move and another AT THE SAME TIME, telling me to move to the right :/
I felt it was essential to voice out that my feet was cold as it meant that blood isnt circulating well to the feet and if I’m in surgery, there might be implications. It was a male person that explained and put on socks for me. I’m thankful.
and then BP cuff, definitely something wasnt right with it. I remember hearing the male anesthesiologist talking about “what is wrong with the BP cuff today”. They tried the same cuff 3 times, and I had pins and needles on my hand, I kept grabbing my left arm to want to indicate something but they didnt respond. I was already on the breathing mask then. Didnt pursue when the male anesthesiologist finally got them to switch to a normal size BP cuff for me. “Shes okay for normal size cuff.” and then I drifted off.
I woke up in the recovery ward, I was itchy on my neck area, I moved my right hand twice to scratch. I still remember myself taking off the pulse monitor on my finger after scratching my neck area the second time and the nurse says I have to keep it on for monitoring. 😀
6:32pm, I got back to my high-dependency ward, I knew because my husband sent the message out on this special occasion group chat. 😀
Dinner was served. I was very hungry… cos I only drank chocolate milk at 7am before coming to the hospital. I only managed 2 sip of soup, 1 small square of carrot and onion. waited with my husband for doctor’s rounds at 9pm. We obediently waited till 9:50pm then they say doctor not coming. :/ hai.
woke up at God knows what time and was really hungry. Requested to eat, they went to heat up the food. GOSH, I didnt even lean forward when the tray was presented to me, the aroma of the food floated to me and I threw up. Into a bag of course.
Turns out it was because of the anesthetic meds. My throat was so bad scratched up and I desperately wanted to drink water, but ya… went to waste. 😀
Finally some time in the middle of the night, I was ushered to go pee, and threw up a little bit, they gave me gastric and anti-vomitting meds. A doctor came and do his rounds. I remember distinctively talking back to the doctor, I repeated his confirmation bias lines to him. He asked if I was feeling well but in a self-confirming manner. I dont remember the exact words. I just repeated what he said to him, adding that I wasnt the one saying that I’m well, he seemed to be the one thats pushing the well respond.
Anyway, I was wheeled to the normal ward the next day, slept till 7:10am ish, was wide awake. Took a walk, took 3 walks around the area. Cant stand lying down, and I know to get well, to leave the hospital, I need to move.
Had a pleasant stay in the wards. Most of the nurses were kind. Perhaps because the post-surgery day was Good Friday so things were not as smooth.
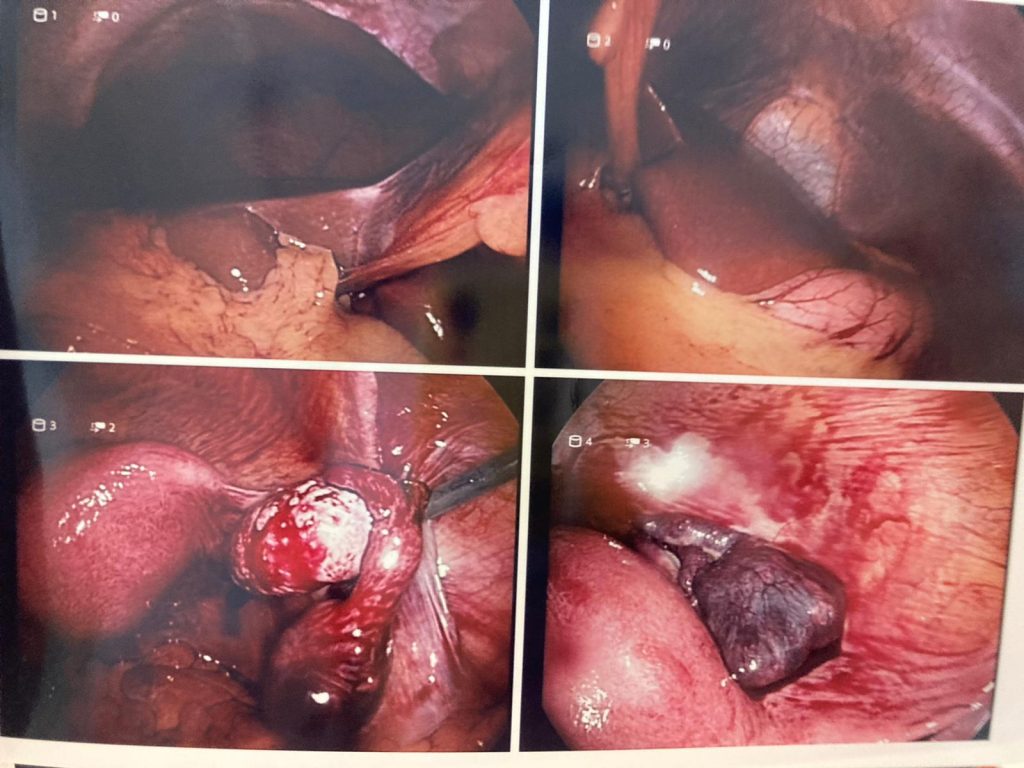
A doctor came and spoke to me about my operation, showed me some photos of what was inside. (Scroll pass the photo quick if you are squirmish.) Bottom left, right ovaries (white part), swollen right fallopian tube. Bottom right, the teddy bear that I won but didnt get to bring back home.
Post-surgery, got a little bit of problem with the slids and dressings, went to the polyclinic, gonna go back to the doctors next week for review.
Life goes on, I’m fine. I even jokingly said give the baby and the tube back to the Lord (since its Good Friday) and He’ll return me new ones. 😀
🙂 Facing life one day at a time.
Thanks for coming by
Be Blessed,
Love,
Amanda